Commercial payers offer varying levels of coverage for family planning services (see the section on coverage for details on requirements). However, patients may not have a clear understanding of the details of their own plan’s coverage. It is a best practice for providers to research the coverage details of various plans and create job aids to provide staff with quickly accessible information. Below is a sample job aid to demonstrate the coverage in different commercial plans.
Patients enrolled in plans subject to the ACA’s contraceptive coverage requirement (see coverage eligibility) cannot be charged a copay for covered contraceptive methods, including LARC, or related counseling, follow-up, side effect management, or removal.
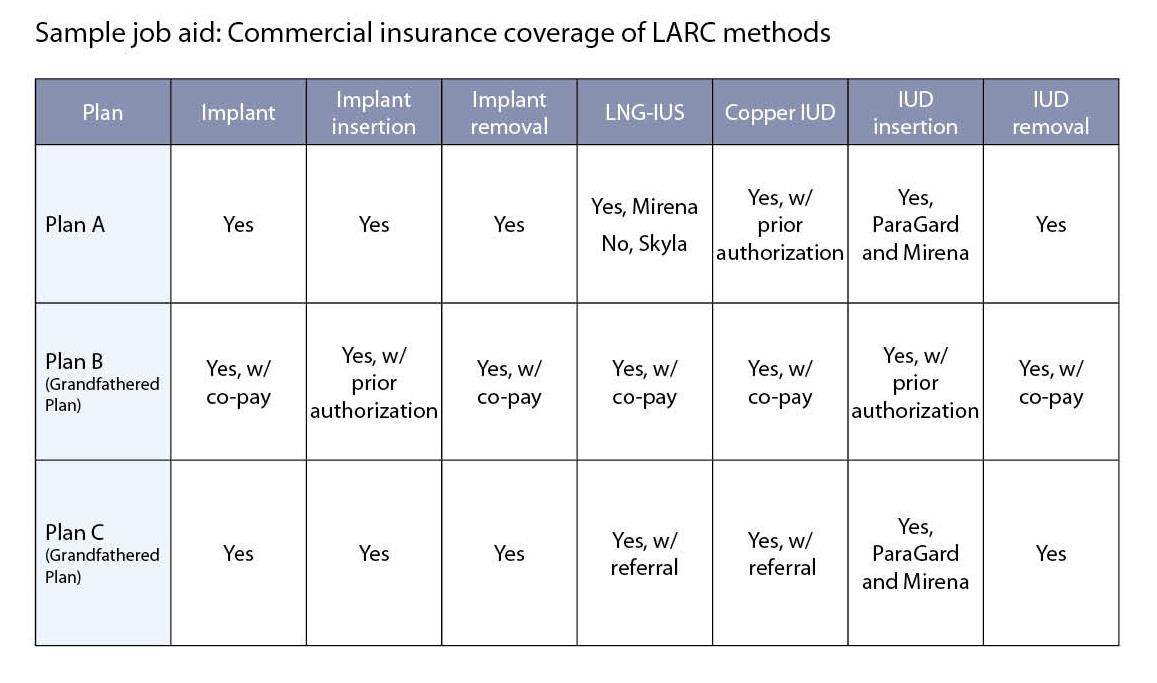
Note: For illustrative purposes only. Coverage varies by plan.
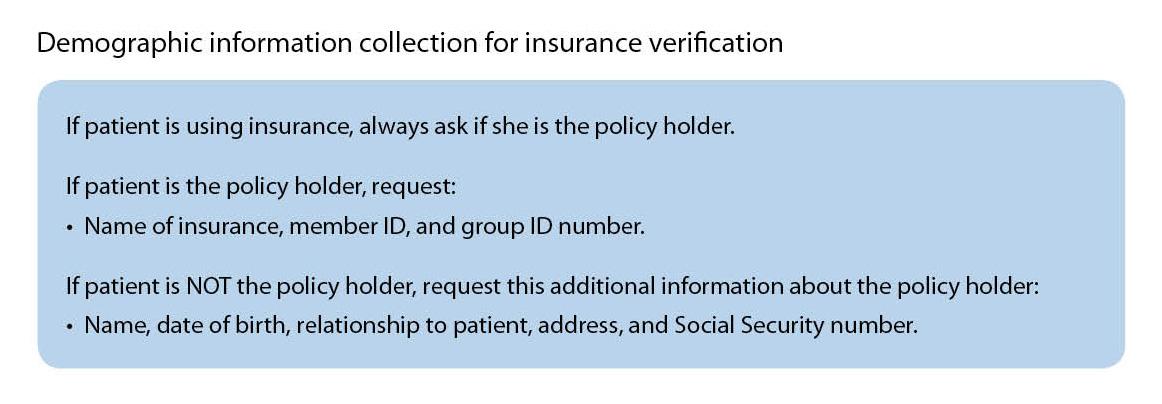
It is in the interest of both the provider and the patient to individually verify a patient’s insurance benefits, preferably before the visit. This process will confirm whether the patient’s coverage is active, as well as any cost-sharing, prior authorization, or referral requirements for LARC methods. Commercial payers are increasingly offering benefit verification online, which can cut down on the amount of time it takes for health center staff to devote to the process. Instantaneous verification also allows staff to confirm insurance benefits even when offering same-day appointment scheduling. A provider should collect the necessary demographic information from the patient included in in the figure below to facilitate benefit verification. Best practices for collecting this information include requesting it from the patient at the time the appointment is made and making a copy of the patient’s insurance benefit card during the appointment.
Manufacturer benefit verification services
Teva Women’s Health offers a benefits verification process specifically for ParaGard through its Access Solutions Program. Providers can register online to gain access to this free program to facilitate patient benefits verification. The turnaround for verification results through this program is usually 24-48 hours.
Bayer offers third-party benefit investigation services at no cost to providers. To gain access to these services, complete the Bayer Women’s HealthCare Support Benefit Investigation Request Form. Benefit investigation results will be provided within 48 hours through a third-party contractor. Curascript provides benefit investigation services for Nexplanon. Call Curascript at 1-866-389-7928 to request a Patient referral form for benefit verification.
Liletta Access Connect offers real-time benefit verification for Liletta though its online portal. To register for the site, a practice must provide its NPI number, clinician license number, basic, contract information, and Medicaid number if applicable. A representative will confirm registration within one business day. After registration is confirmed, log in and click on benefit verification. To complete the formm, a provider will need patient name, date of birth, plan name and member number (see Section 4.3 for more information about collecting benefit verification information). Results should be available immediately; if not, phone support is available on weekdays from 8 am to 8 pm Eastern time at 1-855-545-3882.
If a patient with commercial insurance faces barriers to coverage
The information collected during the benefits verification process can be used to help educate a patient about her coverage and financial responsibility prior to her visit. If a provider discovers that a patient is facing barriers to coverage of LARC methods, the patient should be referred to NWLC’s CoverHer hotline. This hotline provides personalized instructions on how to navigate the health insurance process to ensure women get the coverage for preventive services they are guaranteed under the ACA. Patients can contact CoverHer directly online, at 1-866-745-5487, or [email protected].
Another option for commercially insured patients who want an LNG-IUS but do not have coverage (see the section on coverage eligibility for details on exceptions) is the Liletta Patient Savings Program, which is a form of co-pay assistance. A patient may qualify for this program if she resides in the U.S. or Puerto Rico, has commercial health insurance, has an out-of-pocket expense for a Liletta device greater than $75, and does not participate in any public health insurance plans (e.g. Medicaid).
To help patients use this program, a practice must first register by calling 855-706-4508. The practice is supplied with Liletta Access Cards and patient education materials. The cards function similarly to a debit card, and the amount of money allocated to a card depends on a patient’s out-of-pocket expense for a Liletta. The card will provide a maximum savings of $500. The patient activates the card by going to LilettaCard.com or calling 855-706-4508. Once activated, the card can be used toward the purchase of a Liletta from the practice (if buy and bill), directly from the specialty pharmacy, or to receive a rebate. To obtain a rebate, a patient must have an explanation of benefits form from her health insurance plan and upload it to LilettaCard.com or fax it to 888-683-4991.
Please note that this program does not cover expenses associated with office visits. At the time of publication, this program will expire on September 30th, 2015. Devices must be prescribed in advance of this date to qualify for this program. An EOB must be submitted within 60 days of this date to qualify for a rebate.